BENEFITS, PERSONAL & COMMERCIAL INSURANCE SERVICES
Conner Insurance provides comprehensive commercial, personal, and benefits insurance solutions coverage for people and businesses in all 50 U.S. states. In addition, we understand a company’s most valuable asset is its people, which is why we become your partner, advisor, and supporter. Insurance is complicated, and our team makes the process simple and effective. Schedule a consultation with one of our trusted insurance advisors to learn how our full-service agency can meet your business needs, reduce risk, and maximize your company culture.
Commercial
Our robust insurance solutions cover the entire spectrum of commercial risk management.
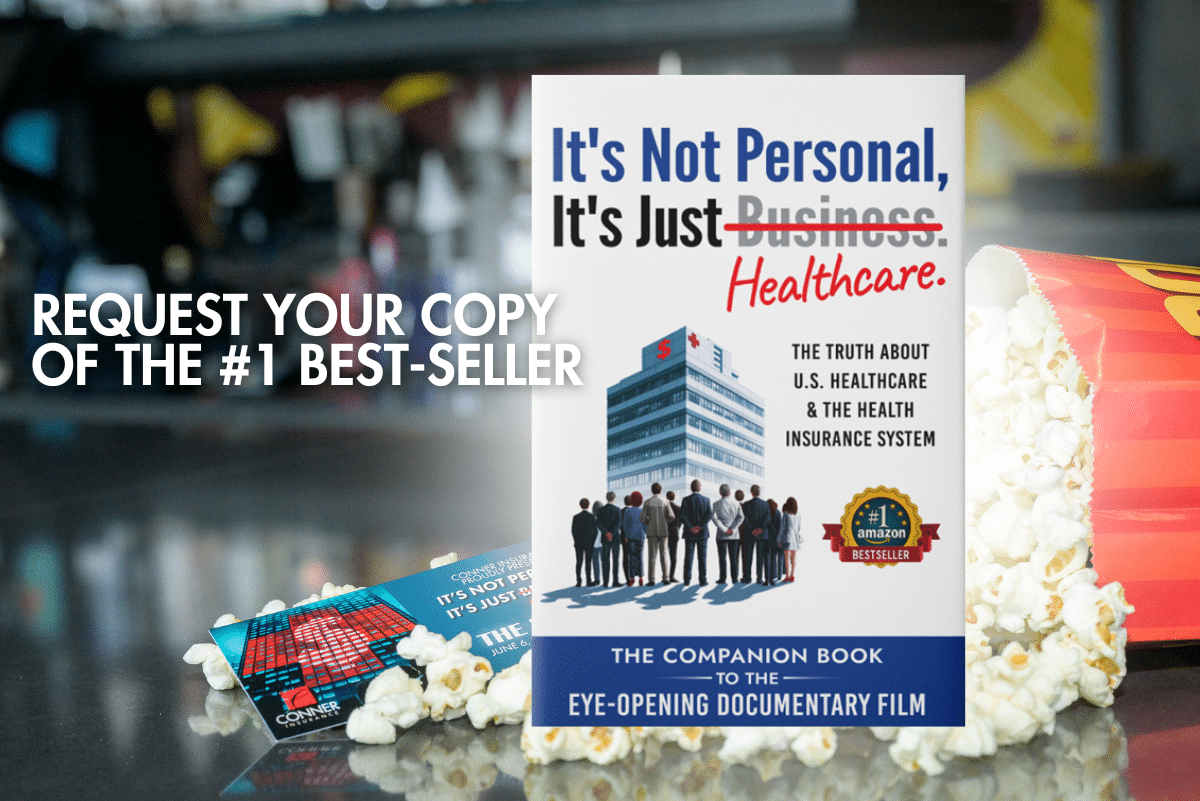
Learn More"It's Not Personal, It's Just Healthcare"
"It's Not Personal, It's Just Healthcare" is an astonishing documentary that Ben Conner has co-produced. It highlights the misaligned incentives in healthcare and sheds light on the fundamental areas that need to be changed to make healthcare affordable for Plan Sponsors.
Watch the Documentary
Our Legacy: 75 Years of Conner Insurance
From a small, family-owned business to a forward-thinking, industry-leading Firm, this video honors the people and moments that shaped who we are today.
Watch the Full Story


 alt="Personal Insurance Solutions">
alt="Personal Insurance Solutions"> alt="Benefits Insurance Solutions">
alt="Benefits Insurance Solutions">